Air Purifiers Help Rhinitis Allergy(1)
The prevalence of allergic rhinitis is increasing year by year, affecting the quality of life of millions of people worldwide.
Air pollution is an important reason for its increased incidence. Air pollution can be classified according to source as indoor or outdoor, primary (emissions directly into the atmosphere such as nitrogen oxides, PM2.5 and PM10) or secondary (reactions or interactions, such as ozone) pollutants.
Indoor pollutants can release a variety of substances harmful to health during heating and cooking, fuel combustion, including PM2.5 or PM10, ozone and nitrogen oxides. Biological air pollution such as mold and dust mites is caused by airborne allergens that can directly lead to atopic diseases such as allergic rhinitis and asthma. Epidemiological and clinical studies have shown that co-exposure to air allergens and pollutants aggravates immune responses and induces inflammatory responses by recruiting inflammatory cells, cytokines, and interleukins. In addition to immunopathogenic mechanisms, rhinitis symptoms can also be mediated by neurogenic components following exposure to environmental stimuli, thereby exacerbating airway reactivity and sensitivity.
Treatment of allergic rhinitis aggravated by air pollution mainly includes treating allergic rhinitis according to guidelines recommended and avoiding exposure to pollutants. Fexofenadine is an antihistamine with selective H1 receptor antagonistic activity. Can improve allergic rhinitis symptoms aggravated by air pollution. More clinical research is needed to clarify the role of other related drugs, such as intranasal corticosteroids, in reducing symptoms caused by co-exposure to air pollution and allergies. In addition to conventional allergic rhinitis drug therapy, careful avoidance measures should be taken to reduce the symptoms of allergic rhinitis and air pollution-induced rhinitis.
Advice for patients
Especially the elderly, patients with severe heart and lung diseases and children in sensitive groups.
• Avoid inhaling tobacco in any form (active and passive)
• Avoid burning incense and candles
• Avoid household sprays and other cleaners
• Eliminate sources of indoor mold spores (moisture damage to ceilings, walls, carpets and furniture) or thoroughly clean with a solution containing hypochlorite
• Replacing daily disposable lenses with contact lenses in patients with conjunctivitis.
• Use of second-generation non-sedating antihistamines or intranasal corticosteroids
• Use anticholinergics when clear watery rhinorrhea occurs
• Rinse with nasal wash to conceptually minimize exposure to contaminants
• Adjust treatments based on weather forecasts and indoor/outdoor pollutant levels, including allergen levels (ie pollen and fungal spores).
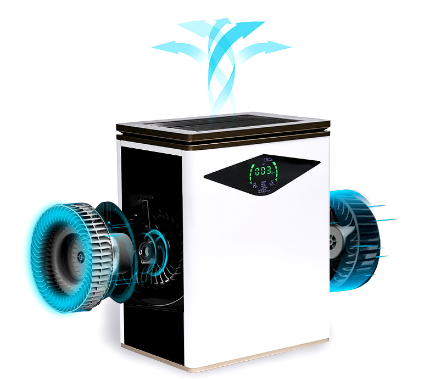
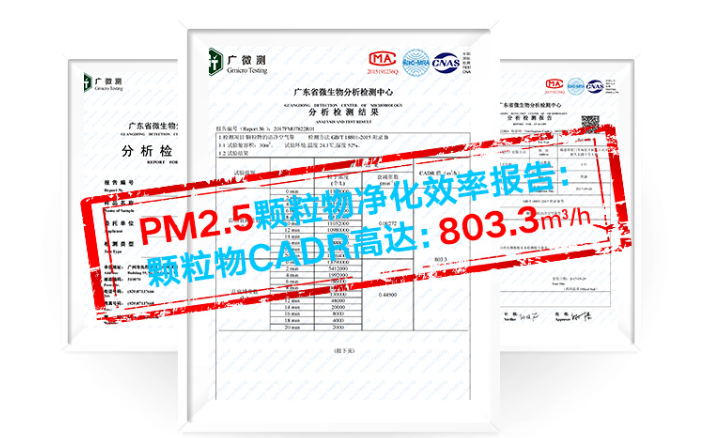
Commercial Air Purifier with turbo fan dual HEPA filtrations